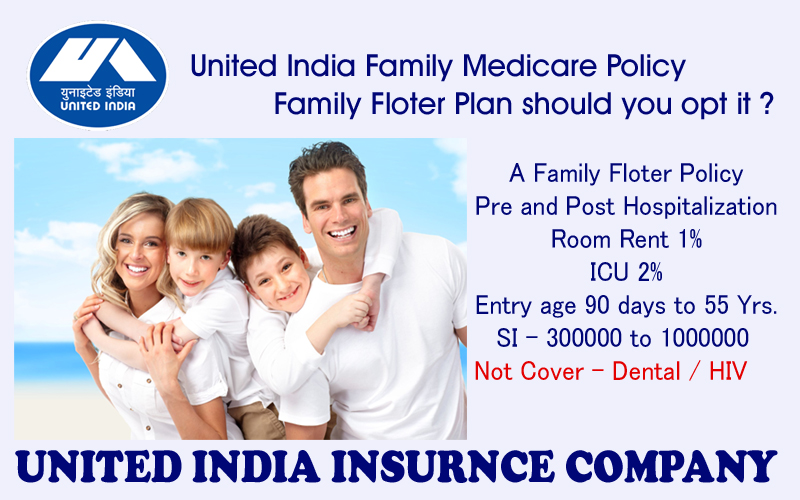
Policy Name : FAMILY MEDICARE POLICY
Policy Code : UIIC001
FAMILY MEDICARE POLICY - PROSPECTUS
SALIENT FEATURES OF THE POLICY
This policy covers all the members of a family under a single sum insured.
Eligibility : Family comprising of Self, Spouse and Dependent Children
Age : Proposer between 18 and 80 years
Dependent children between the age of 3 months and 18 years provided either or both parents are covered concurrently. However, children above 18 years will cease to be covered if they are employed/self-employed or married. For unmarried and unemployed girls, disabled children without income dependent upon Proposer, the age limit of 18 will not apply. Male child upto 26 years can be covered provided they pursue full-time higher studies and submit Bonafide Certificate from Institution.
Sum Insured : Beginning from Rs.1 lac in multiples of Rs.50,000/- upto Rs.5 Lac and from Rs.5 Lac to Rs.10 Lac in multiples of Rs.1 lac.
Existing Individual Health Policyholders of the Company can also opt for Family Medicare Policy on expiry of their current policy if there has been no claim for the preceding two years in respect of insured persons. If parents are covered under existing health policy of the company they can opt for a separate Family Medicare Policy. Either parent or son/daughter can be the proposer for such a policy.
No Claim discount/Cumulative Bonus, if any, under existing policy will not be carried forward.
COVERAGES
Policy covers Hospitalisation Expenses.
Expenses prior to and after hospitalisation are also covered. Further details of coverage are given below:
Expenses on Hospitalisation for minimum period of 24 hours are admissible. However, this time limit is not applied to specific treatments as detailed in the policy.
Note: Procedures/treatments usually done in out patient department are not payable under the policy even if converted as an in-patient in the hospital for more than 24 hours or carried out in Day Care Centres.
Hospitalisation Expenses:
A. Room, Boarding and Nursing Expenses as provided by the Hospital/Nursing Home upto 1% of Sum Insured per day. This also includes Nursing Care, RMO charges, IV Fluids/Blood Transfusion/Injection administration charges and similar expenses.
B. If admitted in IC Unit, the Company will pay upto 2% of Sum Insured per day or actual amount whichever is less.
C. Surgeon, Anaesthetist, Medical Practitioner, Consultants, Specialists Fees
2
D. Anaesthetist, Blood, Oxygen, Operation Theatre Charges, surgical appliances, Medicines & Drugs, Dialysis, Chemotherapy, Radiotherapy, cost of Artificial Limbs, cost of prosthetic devices implanted during surgical procedure like Pacemaker, relevant laboratory diagnostic tests, etc. and other similar expenses.
E. All Hospitalisation Expenses (excluding cost of organ, if any) incurred for donor in respect of Organ transplant to the insured.
Expenses in respect of the following specified surgeries will be restricted as detailed below:
Hospitalisation Benefits
LIMITS FOR EACH HOSPITALISATION
a. Cataract,
b. Hernia,
c. Hysterectomy
d. Following Specified major surgeries
i. Cardiac Surgeries
ii. Cancer Surgeries
iii. Brain Tumour Surgeries
iv. Pacemaker implantation
For sick, sinus syndrome
v. Hip replacement
vi. Knee joint replacement
a. 10% of SI subject to maximum of Rs.25,000/-
b. 15% of SI subject to maximum of Rs.30,000/- .
c. 20% of Sum Insured subject to maximum of Rs.50,000.
d. 70% of the Sum Insured subject to max. Of Rs.4 lac.
The above limits specified are applicable per hospitalisation/ surgery.
Pre & Post Hospitalisation in respect of each hospitalisation
--- Actual expenses incurred subject to maximum of
10% of Sum Insured whichever is less.
In respect of persons above 60 years, 10% deductible will be applied on all admissible claims.
2.1 Expenses on Hospitalisation for minimum period of 24 hours are admissible. However, this time limit is not applied to specific treatments ie.Dialysis, Chemotheraphy, Radiotherapy, eye surgery, dental surgery, Lithotripsy (Kidney Stone removal), Dilatation & Curettage, Tonsilectomy taken in the Hospital/Nursing Home and the insured is discharged on the same day, the treatment will be considered to be taken under hospitalisation benefit.
Further if the treatment /procedure/surgeries of above diseases are carried out, in Day Care Centres which is fully equipped with advanced technology and specialised infrastructure where the insured is discharged on the same day, the requirement of minimum beds will be overlooked provided following conditions are met.
1. The operation theatre is fully equipped for the surgical operation required in
respect of sickness/ailment/injury covered under the policy.
2. Day Care nursing staff is fully qualified.
3. The doctor performing the surgery or procedure as well as post operative attending doctors are also fully qualified for the specific surgery/procedure.
Note: Procedures/treatments usually done in out patient department are not payable under the policy even if converted as an in-patient in the hospital for more than 24 hours
2.2 For Ayuredic Treatment, hospitalisation expenses are admissible only when the treatment has been undergone in a Government Hospital or in any Institute recognised by the Government and/or accredited by Quality Council of India/National Accreditation Board on Health.
MEDICAL EXPENSES INCURRED UNDER TWO POLICY PERIODS
If the claim event falls within two policy periods, the claims shall be paid taking into consideration the available sum insured in the two policy periods, including the deductibles for each policy period. Such eligible claim amount to be payable to the insured shall be reduced to the extent of premium to be received for the renewal/due date of premium of health insurance policy, if not received earlier.
3
DEFINITIONS
3.1 A Hospital means any institution established for in-patient care and day care treatment of illness and/or injuries and which has been registered as a Hospital with the local authorities under the Clinical establishments (Registration and Regulation) Act, 2010 or under the enactments specified under the Schedule of Section 56(1) of the said Act OR complies with all minimum criteria as under
1) Has qualified nursing staff under its employment round the clock.
2) Has at least 10 in-patient beds in towns having a population of less than 10 lacs and at least 15 in-patient beds in all other places;
3) Has qualified medical practitioner(s) in charge round the clock;
4) Has a fully equipped Operation Theatre of its own where surgical procedures are carried out;
5) Maintains daily records of patients and makes these accessible to the insurance company’s authorized personnel.
3.2 Hospitalisation Means admission in a Hospital/Nursing Home for a minimum period of 24 In-patient care consecutive hours except for specified procedures/treatments, where such admission could be for a period of less than 24 consecutive hours.
3.3 ANY ONE ILLNESS
Any one illness will be deemed to mean continuous period of illness and it includes relapse within 45 days from the date of last consultation with the Hospital / Nursing Home where treatment has been taken.
3.4 CASHLESS FACILITY
Cashless facility means a facility extended by the insurer to the insured where the payments, of the costs of treatment undergone by the insured in accordance with the policy terms and conditions, are directly made to the network provider by the insurer to the extent pre-authorisation approved.
3.5 DAY CARE CENTRE
Day Care centre means any institution established for day care treatment of illness and/or injuries or a medical set-up within a hospital and which has been registered with the local authorities, wherever applicable, and is under the supervision of a registered and qualified medical practitioner AND must comply with all minimum criteria as under :
F. Has qualified nursing staff under its employment
G. Has qualified Medical Practitioner(s) in charge
H. Has a fully equipped operation theatre of its own where surgical procedures are carried out-
I. Maintains daily records of patients and will make these accessible to the Insurance Company’s authorized personnel.
3.6 DAY CARE TREATMENT - Day Care treatment means the medical treatment and/or surgical procedure which is – (i). Undertaken under General or Local Anesthesia in a hospital/day care centre in less than 24 hrs because of technological and (ii) which would have otherwise required a hospitalisation of more than 24 hours. Treatment normally taken on an out-patient basis is not included in the scope of this definition.
3.7 GRACE PERIOD
Grace Period means the specified period of time immediately following the premium due date during which a payment can be made to renew or continue a policy in force without loss of continuity benefits such as waiting periods and coverage of pre-existing diseases. Coverage is not available for the period for which no premium is received.
3.8 ID CARD
ID card means the identity card issued to the insured person by the TPA to avail cashless facility in network hospitals.
4
3.9 MEDICALLY NECESARY
Medically Necessary treatment is defined as any treatment, tests, medication, or stay in hospital or part of a stay in hospital which
1. Is required for the medical management of the illness or injury suffered by the insured;
2. Must not exceed the level of care necessary to provide safe, adequate and appropriate medical care in scope, duration or intensity;
3. Must have been prescribed by a Medical Practitioner;
Must conform to the professional standards widely accepted in international medical practice or by the medical community in India.
3.10 MEDICAL PRACTITIONER
A Medical Practitioner is a person who holds a valid registration from the Medical Council of any State of India or Medical Council of India or Council for Indian Medicine or for Homeopathy set up by the Government of India or a State Government and is thereby entitled to practice medicine within its jurisdiction; and is acting within the scope and jurisdiction of licence.
The term Medical Practitioner would include Physician, Specialist and Surgeon. (The Registered Practitioner should not be the insured or close family members such as parents, in-laws, spouse and children).
3.11 NETWORK PROVIDER
Network Provider means the hospital/nursing home or health care providers enlisted by an insurer or by a TPA and insurer together to provide medical services to an insured on payment by a cashless facility. The list of Network Hospitals is maintained by and available with the TPA and the same is subject to amendment from time to time.
Preferred Provider Network means a network of hospitals which have agreed to a cashless packaged pricing for certain procedures for the insured person. The list is available with the company/TPA and subject to amendment from time to time. Reimbursement of expenses incurred in PPN for the procedures (as listed under PPN package) shall be subject to the rates applicable to PPN package pricing.
3.12 PORTABILITY
Portability means transfer by an Individual Health Insurance Policyholder (including family cover) of the credit gained for pre-existing conditions and time-bound exclusions if he/she chooses to switch from one insurer to another.
3.13 PRE-EXISTING DISEASE
Any condition, ailment or injury or relation condition(s) for which you had signs or symptoms, and/or were diagnosed, and/or received medical advice/treatment within 48 months to prior to the first policy issued by the insurer.
3.14 PRE – HOSPITALISATION MEDICAL EXPENSES
Relevant medical expenses incurred immediately 30 days before the Insured person is hospitalised provided that ;
a) Such Medical expenses are incurred for the same condition for which the Insured Person’s Hospitalisation was required; and
b) The In-patient Hospitalisation claim for such Hospitalisation is admissible by the Insurance Company
3.15 POST HOSPITALISATION MEDICAL EXPENSES
Relevant medical expenses incurred immediately 60 days after the Insured person is discharged from the hospital provided that ;
a. Such Medical expenses are incurred for the same condition for which the Insured Person’s Hospitalisation was required; and
b. The In-patient Hospitalisation claim for such Hospitalisation is admissible by the Insurance Company.
3.16 QUALIFIED NURSE
QUALIFIED NURSE means a person who holds a valid registration from the Nursing Council of India or the Nursing Council of any State in India.
5
3.17 REASONABLE AND CUSTOMARY CHARGES
Reasonable and Customary charges means the charges for services or supplies, which are the standard charges for the specific provider and consistent with the prevailing charges in the geographical area for identical or similar services, taking into account the nature of illness/injury involved.
3.18 THIRD PARTY ADMINISTRATOR
TPA means a Third Party Administrator who holds a valid License from Insurance Regulatory and Development Authority to act as a THIRD PARTY ADMINISTRATOR and is engaged by the Company for the provision of health services as specified in the agreement between the Company and TPA.
EXCLUSIONS:-
Any pre-existing condition(s) as defined in the policy, until 48 months of continuous coverage of such insured person have elapsed, since inception of his/her first policy as mentioned in the schedule of the policy.
N.B.: A Pre-existing disease is defined as “any condition, ailment or injury or related condition(s) for which insured person had signs or symptoms, and /or was diagnosed and/or received medical advice/treatment within 48 months prior to his/her first policy as mentioned in the schedule of the policy”.
Any disease contracted by the Insured person during the first 30 days from the commencement date of the policy. This does not apply if the person has been insured for the twelve months immediately preceding the commencement of this Policy.
Unless the Insured has 24 months of continuous coverage, the expenses on treatment of diseases such as Cataract, Benign Prostatic Hyperthrophy, Hysterectomy for Menorrhagia or Fibromyoma, Hernia, Hydrocele, Congenital internal disease, Fistula in anus, piles, Sinusitis and related disorders, Gall Bladder Stone removal, Gout & Rheumatism, Joint Replacement due to Degenerative Condition and age-related Osteoarthiritis & Osteoporosis are not payable.
Injury / disease directly or indirectly caused by or arising from or attributable to invasion, Act of Foreign enemy, War like operations (whether war be declared or not)
a. Circumcision unless necessary for treatment of a disease not excluded hereunder or as may be necessitated due to an accident.
b. vaccination or inoculation of any kind unless it is post animal bite, change of life or cosmetic or aesthetic treatment of any description such as correction of eyesight, etc.
c. plastic surgery other than as may be necessitated due to an accident or as a part of any illness.
Cost of spectacles, contact lenses and hearing aids.
Dental treatment or surgery of any kind unless necessitated by accident and requiring hospitalisation.
Convalescence, general debility; run-down condition or rest cure, Congenital external disease/defects or anomalies, Sterility, Venereal disease, intentional self injury and use of intoxication drugs / alcohol
All expenses arising out of any condition directly or indirectly caused to or associated with Human T-Cell Lymphotropic Virus Type III (HTLB - III) or lymphadenopathy Associated Virus (LAV) or the Mutants Derivative or Variation Deficiency Syndrome or any syndrome or condition of a similar kind commonly referred to as AIDS.
Charges incurred at Hospital or Nursing Home primarily for diagnosis.
Expenses on vitamins and tonics unless forming part of treatment.
Injury or Disease directly or indirectly caused by or contributed to by nuclear weapon / materials
Treatment arising from or traceable to pregnancy (including voluntary termination of pregnancy) and childbirth (including caesarean section).
Naturopathy Treatment, acupressure, acupuncture, magnetic and such other therapies.
External and or durable Medical / Non-medical equipment of any kind used for diagnosis and/or treatment and/or monitoring and/or maintenance and/or support including CPAP,
6
CAPD, Infusion Pump, Oxygen Concentrator etc., Ambulatory devices ie. walker, crutches, Belts, Collars, Caps, Splints, Slings, Braces, Stockings, etc. of any kind, Diabetic footwear, Glucometer/ Thermometer, and similar related items and also any medical equipment, which are subsequently used at home.
Any kind of Service charges, Surcharges, Admission Fees/Registration Charges, levied by the hospital.
All non-medical expenses of any kind whatsoever, for detailed list, please visit our website www.uiic.co.in.
PROCEDURE FOR TAKING A POLICY
The duly completed and signed Proposal form giving details of all Insured persons and a signed copy of the Prospectus along with Health Check-up reports, if any, should be submitted to the Company.
The pre-acceptance health check-up reports as detailed below have to be submitted at proposer’s cost in the following cases–
i. Persons above 45 years of age (fresh entrants)
ii. Persons above 45 years of age (Break in insurance)
iii. Persons above 45 years of age and seeking enhancement of Sum Insured of Family Medicare Policy by more than two slabs.
iv. Our Existing policyholders above 45 years opting for Sum Insured under Family Medicare Policy which is more than twice the maximum existing individual Sum Insured.
1 Medical Examination 6. Sr.Creatinine
2 CBC & ESR 7. ECG
3 Urine Routine & Microscopic 8. Stress Test
4 Cholesterol
5 SGPT
NOTE : 50% of the cost of Health check-up shall be reimbursed to the Insured in cases where the proposal is accepted by the Company.
The insured should declare the existence of Diabetes, Hypertension, Elevated Cholesterol level, if any, at the time of taking the first policy. The policy will not pay for the expenses incurred for the direct treatment of these illnesses as per Pre-existing Disease exclusion. An additional premium of 30% will be charged on the basic premium.
PAYMENT OF PREMIUM : As per table attached.
Age of the oldest person of the family is considered while referring to the Premium table.
The Policy shall be void and all premium paid hereon shall be forfeited to the Company, in the event of misrepresentation, mis-description or non-disclosure of any material fact.
RENEWAL
1. The Company shall renew this policy if the insured shall remit the requisite premium to the Company prior to expiry of the period of insurance stated in the schedule.
2. The Company shall be entitled to decline renewal if;
a. Any fraud, misrepresentation or suppression by the insured or on his behalf is found either in obtaining insurance or subsequently in relation thereto or,
b. The Company has discontinued issue of the policy, in which event the insured shall however have the option for renewal under any similar policy being issued by the company, provided however benefits payable shall be subject to the terms contained in such other policy.
3. If the insured fails to remit premium for renewal before expiry of the period of insurance, but within 30 days thereafter, admissibility of any claim during the period of subsequent policy shall be considered in the same manner as under a Policy renewed without break. The Company however shall not be liable for any claim arising out of ailment suffered or
7
hospitalisation commencing in the interim period after expiry of the earlier policy and prior to date of commencement of subsequent policy.
4. The insured may seek enhancement of Sum Insured in writing at or before payment of premium for renewal, which may be granted at the discretion of the Company. However, notwithstanding enhancement, for claims arising in respect of ailment, disease or injury contracted or suffered during a preceding policy period, liability of the company shall be only to the extent of the Sum Insured under the policy in force at the time when it was contracted or suffered.
Any such request for enhancement must be accompanied by a declaration that the insured or any other insured person in respect of whom such enhancement is sought is not aware of any symptoms or other indications that may give rise to a claim under the policy. The Company may require such insured person/s to undergo a Medical examination to enable the company to take a decision on accepting the request for enhancement in the Sum Insured. 50% of the cost of the Medical examination will be reimbursed to the insured person on acceptance of the request for enhancement of sum insured.
PORTABILITY
In the event of insured porting to another insurer, the insured person must apply with details of policy and claims at least 45 days before the date of expiry of policy.
Portability shall be allowed in the following cases :
a. All Individual Health Insurance Policies issued by non-life insurance companies including family floater policies.
b. Individual members, including the family members covered under any Group Health insurance policy of a non-life insurance company shall have the right to migrate from such a group policy to an individual health insurance policy or a family floater policy with the same insurer. One year thereafter, the insured person shall be accorded the right to port to another non-life insurance company.
NO CLAIM DISCOUNT/CLAIMS LOADING
At renewal, the Company will review the claims experience and apply a No Claim Discount/Loading based on the claims incurred as given below.
No Claim Discount – 3% on renewal premium after three continuous claim free Family Medicare Policies and for every subsequent claim free year subject to a maximum of 15%.
If any claim is reported or if the policy is not renewed within the grace period, the Policy will not be eligible for any No Claim discount.
TAX REBATE
Tax rebate available as per provision of Income Tax rules under Section 80-D.
FREE LOOK PERIOD
The policy have a free look period which shall be applicable at the inception of the policy and;
i. The insured will be allowed a period of at least 15 days from the date of receipt of the policy to review the terms and conditions of the policy and to return the same if nor acceptable.
ii. If the insured has not made any claim during the free look period, the insured shall be entitled to –
a. A refund of the premium paid less any expenses incurred by the insurer on medical examination of the insured persons and the stamp duty charges or
b. Where the risk has already commenced and the opinion of return of the policy is excercised by the policybolder, a deduction towards the proportionate risk premium for period on cover or;
c. Where only a part of the risk has commenced, such proportionate risk premium commensurate with the risk covered during such period
HEALTH CHECK-UP BENEFIT
8
For every block of three claim free years, the insured person(s) will be eligible for Cost of Health check-up up to a maximum of 1% of average SI of preceding three years.
OPTIONAL COVERS
The following optional covers are available on payment of additional premium as given below
1 Ambulance Charges
The Policy will cover Ambulance charges in connection with admitted claim incurred to shift the insured person from Residence/accident site to Hospitals in emergency cases and from one Hospital/Nursing Home to another Hospital/Nursing Home/Diagnostic centre for better care/diagnosis, upto a maximum of Rs.2500/- per policy period – Additional Premium Rs.100/-.
2 Hospital Daily Cash Benefit
The Policy will pay to the insured person a Daily Cash Allowance as given below from the third day onwards for the period of hospitalisation in connection with admitted claims subject to a maximum stated below on payment of additional premium as under –
Additional Premium Allowance per day Subject to maximum of
Rs.150/- Rs.250/- Rs.2,500/- per policy period
Rs.300/- Rs.500/- Rs.5,000/- per policy period
CLAIM PROCEDURE
All claims will be processed and settled by specified Third Party Administrator (TPA) licensed by IRDA.
The payment will be made either to Hospital/Nursing Home in case of Cashless treatment and to the Proposer/insured person in other cases.
Intimation of Hospitalisation– to be made immediately to the TPA.
To avail Cashless facility - Pre-authorisation request to be sent or faxed to TPA immediately on admission.
In Reimbursement cases – Insured to intimate TPA about hospitalisation of insured persons immediately on admission or not later than 24 hours.
Claim bills to be submitted to TPA within fifteen days of discharge.
All claims under this policy shall be payable in Indian currency.
CANCELLATION
The Company may at any time cancel the Policy on grounds of misrepresentation, fraud, non-disclosure of material fact or non-cooperation by the insured by sending fifteen days notice in writing by Registered A/D to the insured at his last known address in which case the Company shall return to the insured a proportion of the last premium corresponding to the unexpired period of insurance if no claim has been paid under the policy.
The insured may at any time cancel this policy and in such event the Company shall allow refund of premium at Company’s short period rate table given below provided no claim has occurred upto the date of cancellation.
PERIOD ON RISK RATE OF PREMIUM TO BE CHARGED.
Upto one month 1/4 th of the annual rate
Upto three months 1/2 of the annual rate
9
Upto six months 3/4th of the annual rate
Exceeding six months Full annual rate.
GRIEVANCE REDRESSAL : In the event of the policyholder having any grievance relating to the insurance, the insured person may submit in writing to the Policy Issuing Office or Grievance cells at Regional Office of the Company for redressal. If the grievance remains unaddressed, the insured person may contact the Officer, Uni-Customer Care Department, Head Office.
OMBUDSMAN
The Insured person can also approach the office of Insurance Ombudsman of the respective area/region for redressal of grievance. The updated list of office of Insurance Ombudsman are available on IRDA website www.irda.gov.in and on the website of General Insurance Council www.gicouncil.in
The Company may revise any of the terms, conditions and exceptions of this insurance including the premium payable on renewal in accordance with the guidelines/rules framed by the Insurance Regulatory and Development Authority (IRDA) and after obtaining prior approval from the Authority. We shall notify you of such changes at least three months before the revision are to take effect.
The Company may also withdraw the insurance as offered hereunder after following the due process as laid down by the IRDA and after obtaining prior approval of the Authority and we shall offer to cover you under such revised/new terms, conditions, exceptions and premium for which we shall have obtained prior approval from the Authority.
This Prospectus shall form part of the proposal form. Please sign in token of having noted the contents of Prospectus.
For full details, please log on to www.uiic.co.in or visit our office.
Signature
Name
Place
Date